What is revenue cycle management (RCM)? Simply put, RCM is the financial process that healthcare organizations use to manage patient care episodes from registration and appointment scheduling to the final payment of a balance. It encompasses the identification, management, and collection of patient revenue, ensuring that healthcare providers are properly reimbursed for the services they render. By integrating RCM with medical billing processes, healthcare organizations can streamline their financial operations, improve cash flow, and maintain financial stability.
Understanding Revenue Cycle Management (RCM)
Revenue cycle management (RCM) in healthcare is a complex and multifaceted process that involves the management of patient revenue from the moment a patient schedules an appointment until the final payment is collected. RCM is crucial for the financial viability of healthcare organizations, as it directly impacts their ability to generate revenue and maintain a healthy cash flow.
The significance of RCM in healthcare administration cannot be overstated. Effective RCM processes ensure that healthcare providers are properly reimbursed for the services they provide, minimizing the risk of lost revenue due to claim denials, delayed payments, or uncollected patient balances. By optimizing RCM, healthcare organizations can improve their financial performance, reduce administrative burden, and allocate more resources to patient care.
Moreover, RCM plays a vital role in ensuring compliance with various healthcare regulations and guidelines. Proper documentation, coding, and billing practices are essential to avoid legal and financial repercussions. RCM helps healthcare organizations navigate the intricacies of insurance reimbursements, government regulations, and patient billing, thereby minimizing the risk of non-compliance and ensuring the organization’s long-term success.
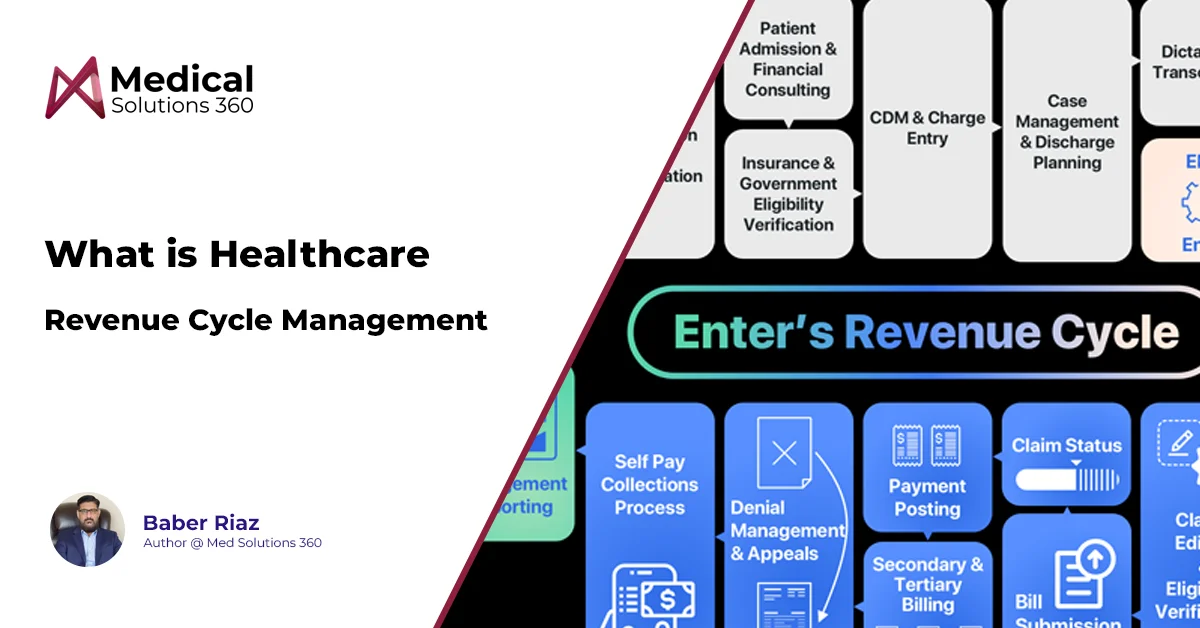
The Lifecycle of Revenue Cycle Management
The revenue cycle management process consists of several key stages, each playing a crucial role in ensuring the smooth flow of patient revenue. From pre-registration to account resolution, understanding the lifecycle of RCM is essential for healthcare organizations seeking to optimize their financial performance
A. Pre-Registration and Registration
The pre-registration and registration stage is the foundation of the revenue cycle management process. Accurate patient information and insurance verification are critical to ensure proper billing and reimbursement. During this stage, healthcare organizations collect vital data, such as patient demographics, insurance coverage, and medical history. By verifying insurance eligibility and benefits upfront, providers can minimize the risk of claim denials and delayed payments downstream.
B. Charge Capture and Coding
Charge capture and coding are essential components of the RCM lifecycle. Medical coding involves the translation of healthcare diagnoses, procedures, and services into universal alphanumeric codes, such as ICD-10, CPT, and HCPCS. Accurate coding is crucial for proper reimbursement, as it determines the amount of payment healthcare organizations receive from insurance payers. Efficient charge capture processes ensure that all billable services are documented and coded correctly, minimizing the risk of lost revenue.
C. Claim Submission and Management
Once charges are captured and coded, the next step in the RCM lifecycle is claim submission. Healthcare organizations must submit claims to insurance payers in a timely and accurate manner, following the specific requirements and guidelines set by each payer. Effective claim management involves monitoring the status of submitted claims, identifying and correcting errors, and appealing denied claims when necessary. Compliance with payer policies and regulations is essential to avoid delays in payment and minimize the risk of denials.
D. Remittance Processing and Insurance Follow-Up
Remittance processing and insurance follow-up are critical stages in the RCM lifecycle. When insurance payers process claims, they send back remittance advice, which includes information on payment amounts, adjustments, and denials. Healthcare organizations must carefully review and reconcile these remittances to ensure accurate payment posting and identify any discrepancies. Insurance follow-up involves communicating with payers to resolve issues, appeal denials, and obtain proper reimbursement for services rendered.
E. Patient Billing and Account Resolution
The final stage of the RCM lifecycle focuses on patient billing and account resolution. After insurance payments have been posted, healthcare organizations must generate and send patient statements for any remaining balances. Effective patient billing strategies involve clear communication, flexible payment options, and prompt follow-up on outstanding balances. Account resolution requires diligent efforts to collect patient payments, negotiate payment plans, and minimize the risk of bad debt. By implementing patient-friendly billing practices and proactive account resolution techniques, healthcare organizations can improve patient satisfaction and maintain a healthy revenue stream.
Key Components of an Effective RCM System
An effective revenue cycle management system is essential for healthcare organizations to streamline their financial processes and optimize revenue collection. Two key components of a successful RCM system are the integration of electronic health records (EHR) and the utilization of advanced technologies, such as artificial intelligence (AI) and machine learning.
EHR integration is crucial for seamless data flow and improved accuracy throughout the RCM process. By connecting EHR systems with RCM software, healthcare organizations can ensure that patient information, clinical data, and billing codes are consistently and accurately captured. This integration reduces the risk of manual errors, improves data integrity, and enables real-time updates across the revenue cycle.
AI and machine learning are transformative technologies that are revolutionizing the RCM landscape. These intelligent systems can automate and optimize various aspects of the revenue cycle, from coding and claim submission to denials management and payment posting. AI-powered RCM solutions can analyze vast amounts of data, identify patterns, and make predictions, enabling healthcare organizations to make data-driven decisions and improve financial performance. Machine learning algorithms can continuously learn and adapt, enhancing the accuracy and efficiency of RCM processes over time.
Challenges in Revenue Cycle Management
Despite the critical importance of revenue cycle management, healthcare organizations often face numerous challenges that can hinder their financial performance and operational efficiency. Some common RCM challenges include:
- Coding and billing errors: Inaccurate coding and billing can lead to claim denials, delayed payments, and lost revenue.
- Inefficient processes: Manual and fragmented RCM processes can result in lengthy payment cycles, increased administrative burden, and higher operational costs.
- Changing regulations: Keeping up with the constantly evolving healthcare regulations and payer requirements can be challenging and time-consuming.
- Lack of staff expertise: Inadequate training and high turnover rates can lead to a lack of skilled RCM professionals, impacting the quality and consistency of RCM processes.
To overcome these challenges, healthcare organizations must adopt a multifaceted approach that includes leveraging technology, investing in staff training, and implementing best practices.
Embracing advanced RCM technologies, such as automation, AI, and machine learning, can significantly reduce manual errors, streamline processes, and improve overall efficiency. These technologies can help organizations keep pace with regulatory changes and adapt to new requirements more effectively.
Benefits of Effective Revenue Cycle Management
Implementing an effective revenue cycle management system offers numerous benefits to healthcare organizations, positively impacting their financial performance, patient satisfaction, and overall operational efficiency.
Improving financial performance and cash flow
One of the primary benefits of effective RCM is the improvement in financial performance and cash flow. By streamlining the revenue cycle process, healthcare organizations can minimize claim denials, reduce accounts receivable days, and accelerate payment collection. This leads to a more stable and predictable revenue stream, enabling organizations to better manage their financial resources and invest in growth opportunities.
Reducing claim denials and rejections
Effective RCM practices significantly reduce the incidence of claim denials and rejections. By ensuring accurate coding, complete documentation, and timely submission of claims, healthcare organizations can minimize the risk of payer denials. This not only improves the organization’s financial performance but also reduces the administrative burden associated with reworking and resubmitting denied claims.
Enhancing patient satisfaction and experience
A well-managed revenue cycle can greatly enhance patient satisfaction and experience. By providing clear and accurate billing information, offering flexible payment options, and promptly addressing patient concerns, healthcare organizations can build trust and loyalty among their patient population. Improved patient satisfaction can lead to increased patient retention, positive word-of-mouth referrals, and a stronger reputation in the community.
Ensuring compliance with regulations and guidelines
Effective RCM helps healthcare organizations maintain compliance with the ever-changing regulatory landscape. By implementing processes that adhere to industry standards, such as HIPAA, ICD-10, and payer-specific guidelines, organizations can avoid costly penalties and legal issues. Compliance also ensures that the organization is properly reimbursed for the services provided, minimizing the risk of lost revenue due to non-compliance.
Optimizing staff productivity and efficiency
An efficient RCM system optimizes staff productivity and efficiency by automating routine tasks, reducing manual errors, and streamlining workflows. This allows RCM professionals to focus on high-value activities, such as denials management, patient communication, and process improvement. By leveraging technology and implementing best practices, healthcare organizations can maximize the productivity of their RCM team, leading to improved financial outcomes and increased job satisfaction.
The Future of RCM in Healthcare
As the healthcare industry continues to evolve, the future of revenue cycle management is closely tied to the adoption of cutting-edge technologies and the ability to adapt to emerging trends. Artificial intelligence (AI), natural language processing (NLP), and blockchain are among the most promising technologies that are expected to revolutionize RCM in the coming years.
AI and NLP have the potential to transform the way healthcare organizations manage their revenue cycle. These technologies can automate complex tasks, such as coding and claims processing, reducing the risk of human error and improving efficiency. AI-powered systems can analyze vast amounts of data, identify patterns, and make intelligent decisions, enabling healthcare organizations to optimize their revenue cycle performance. NLP can extract valuable insights from unstructured data, such as clinical notes and patient feedback, helping organizations to improve the accuracy of their coding and billing processes.
Blockchain technology is another exciting development that could have a significant impact on RCM in healthcare. By creating a secure, decentralized ledger of financial transactions, blockchain can increase transparency, reduce fraud, and streamline payment processes. This technology has the potential to revolutionize the way healthcare organizations manage their financial data, enabling seamless integration between providers, payers, and patients.
As the healthcare landscape evolves, RCM practices will need to adapt to new payment models, such as value-based care and population health management. Healthcare organizations will need to focus on delivering high-quality, cost-effective care while ensuring the financial sustainability of their operations. This will require a data-driven approach to RCM, leveraging advanced analytics and predictive modeling to identify opportunities for improvement and optimize financial performance.
RCM Best Practices for Medical Billing
To optimize their revenue cycle management processes, healthcare providers should adopt a range of best practices and strategies. These include:
- Accurate coding: Ensuring that all medical services are accurately coded using the latest ICD-10, CPT, and HCPCS codes is essential for proper reimbursement and compliance.
- Claim management: Implementing a robust claim management process, including real-time eligibility verification, claim scrubbing, and denial management, can help minimize claim rejections and improve payment collection.
- Patient communication: Providing clear, timely, and accurate communication to patients regarding their financial responsibilities, payment options, and account status can help improve patient satisfaction and reduce the risk of bad debt.
- Staff training: Investing in ongoing training and education for RCM staff is crucial to ensure they have the knowledge and skills necessary to navigate the complexities of medical billing and coding.
- Technology adoption: Embracing advanced technologies, such as automation, AI, and machine learning, can help streamline RCM processes, reduce manual errors, and improve overall efficiency.
- Performance monitoring: Regularly monitoring key performance indicators (KPIs), such as claim denial rates, days in accounts receivable, and net collection ratio, can help identify areas for improvement and track progress over time.
Wrapping Up
By understanding the key components of RCM, leveraging advanced technologies, and implementing best practices, healthcare providers can optimize their financial performance, improve patient satisfaction, and ensure compliance with industry regulations. As the healthcare industry continues to evolve, staying attuned to emerging trends and adopting a proactive approach to RCM will be essential for long-term success. If you are interested in learning more about how to optimize your organization’s revenue cycle management processes, consider exploring the services offered by MedSolutions360.com. Our team of experienced professionals can help you navigate the complexities of RCM and implement tailored solutions to improve your financial performance and drive sustainable growth.